Patient assistance programs also help patients access the most effective, cutting-edge treatments. A 2018 study by the USC Schaeffer Center for Health Policy & Economics found that a majority of co-pay assistance was directed to patients seeking treatments for which there was no generic substitute
Full Answer
What is a patient assistance program (PAP)?
Patient assistance programs (PAPs) help people with no health insurance and those who are underinsured afford medications. These programs are managed by pharmaceutical companies, nonprofits, and government agencies. PAPs may cover the full cost of medications or provide a discount.
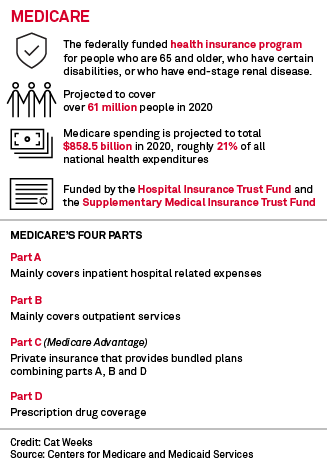
How do Medicare savings programs pay for premiums?
premiums through a Medicare Savings Program. If you qualify, Medicare Savings Programs might also pay your Part A and Part B deductibles, coinsurance, and copayments. You’ll apply for Medicare Savings Programs through your state. When you apply, your state determines which program (s) you qualify for.
Who pays for prescription drug assistance?
These programs are managed by pharmaceutical companies, nonprofits, and government agencies. PAPs may cover the full cost of medications or provide a discount. Many Americans are partially shielded from the high cost of prescription drugs through employer health insurance, Medicaid, or Medicare.
How do I sign up for a medication assistance program?
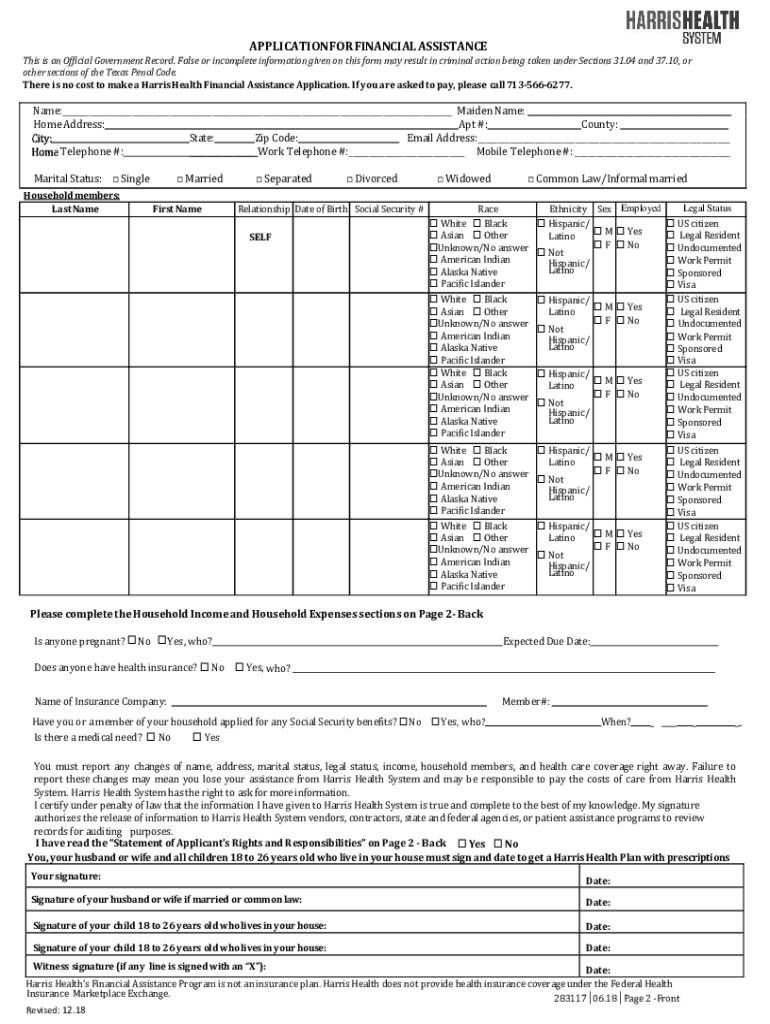
To sign up, you will either call the program or register online. You will need to submit forms like your tax documents and proof of residence to prove your eligibility. Most programs also require your healthcare provider to fill out a form. Once you are enrolled, there may be limits on how much medication you can get or how long the program lasts.
Why do pharmaceutical companies offer patient assistance programs?
Patient assistance programs (PAPs) are usually sponsored by pharmaceutical manufacturers and are promoted as a safety net for Americans who have no health insurance or are underinsured. The goal of these programs is to provide financial assistance to help these patients access medications for little or no cost.
What is patient assist?
Pharmaceutical manufacturers may sponsor patient assistance programs (PAPs) that provide financial assistance or drug free product (through in-kind product donations) to low income individuals to augment any existing prescription drug coverage.
Can you use copay assistance with Medicare?
The Patient Advocate Foundation (PAF) Co-Pay Relief Program (CPR) provides direct financial support for pharmaceutical co-payments to insured patients, including Medicare Part D beneficiaries, who financially and medically qualify.
What is the South Carolina prescription assistance program?
The South Carolina Drug Card is a program provided to you and your family to help lower your prescription drug costs. Simply create and print your FREE Prescription Drug Card below and receive savings of up to 75% (discounts average roughly 30%) at more than 56,000 national and regional pharmacies.
What is patient care support services?
What is Patient Care Assistance? Patient care assistants help provide care, support, and services to patients in a hospital or health care environment. Patient care assistants constantly work under the direction and supervision of nurses and patient support service managers as part of a team.
What does patient support include?
Patient Support Programs (PSPs) are an umbrella term to describe initiatives led by pharmaceutical companies to improve access, usage, and adherence to prescription drugs. These programs can have a financial component, support clinical investments, focus purely on education, or a combination.
Can a provider waive a Medicare copay?
If a Medicare carrier becomes aware that a provider routinely waives the collection of copayment amounts for Medicare beneficiaries, except for amounts deemed too small to warrant collection efforts or where documentation of hardship and indigence is established, the carrier is instructed to determine whether the ...
Does Medicare Part B pay for copays?
There are generally no copayments with Original Medicare — Medicare Part A and Part B — but you may have coinsurance costs. You may have a copayment if you have a Medicare Advantage plan or Medicare Part D prescription drug plan. The amount of your copayment in those cases varies from plan to plan.
What is the Medicare donut hole for 2022?
You enter the donut hole when your total drug costs—including what you and your plan have paid for your drugs—reaches a certain limit. In 2022, that limit is $4,430.
What drugs does Paad cover?
PAAD provides coverage for prescribed legend drugs, insulin and insulin supplies, and needled and syringes for injectable medicines used for the treatment of multiple sclerosis. The PAAD co-payment will be $5 for each PAAD covered generic drug prescription and $7 for each PAAD covered brand name drug prescription.
Is prescription hope based on income?
With respect to Prescription Hope's simple eligibility guidelines, individuals need to earn $32,000 per year or less, or have a combined household income of $50,000 per year or less.
Is prescription assistance services legitimate?
Some people ask us if the prescription assistance programs that we work with are a scam. Prescription assistance programs are a legitimate solution for many Americans that wish to save money on their medical bills. Most prescription assistance programs are offered directly by manufacturers of the brand name medication.
What do patient support assistants do?
Patient support assistants are healthcare professionals who work with patients to ensure that they have everything they need while in the hospital. They may help them with basic needs like bathing, dressing, and eating, but they also provide emotional support and assistance with daily activities.
What are the role and functions of a patient care assistant explain?
observing, monitoring and recording patients' conditions by taking temperatures, pulse, respirations and weight. communication with patients, relatives and carers. assisting with clinical duties. personal care including infection prevention and control, food, personal hygiene and overall reassurance, comfort and safety.
What is the role of patient services?
A Patient Service Representative is a professional responsible for scheduling patient appointments and making reminder calls to patients. They inform patients about delays or wait times to ensure they are seen on time while also updating their information at every visit.
Why are patient care assistants important?
They provide direct care to patients, often assisting them with daily activities like bathing, dressing, eating, etc. They may also help with more complex tasks like transferring from one bed or chair to another, administering medications, and performing other duties as directed by a nurse or doctor.
What is the focus of PAPs?
Ultimately, data sharing and communication between charity PAPs and donors appears to be the key area of focus for OIG, DOJ, and IRS enforcement. If such communication and data sharing is prohibited, whether by state statute or federal regulatory enforcement, it is remains to be seen whether PAPs will continue to operate as they are currently structured. In any event, it is incumbent upon interested parties to stay abreast of changes in the law and developing enforcement trends, and to continually monitor and update their compliance programs accordingly. For example, given the amount of scrutiny applied to coordination between the business and charitable giving arms of medical product manufacturers, compliance programs should be actively examining all intra-firm transactions to assure that no improper influence is being exerted over communications with and donations to charity PAPs.
What is the purpose of PAPs?
Department of Health and Human Services (“HHS”) Office of the Inspector General (“OIG”) has continually acknowledged that properly structured PAPs can provide important “safety net assistance” to patients with limited financial means who cannot afford necessary drugs. This Client Alert provides a comprehensive review ...
What should stakeholders do with PAPs?
Stakeholders should also closely monitor federal and state legislative policy developments regarding PAPs, including copayment assistance and product coupons. K&L Gates regularly advises clients on health care fraud and abuse risk mitigation and compliance matters and facilitate stakeholder engagement with Congress and state legislators and HHS.
What are the two aspects of PAP?
The OIG has indicated that PAPs generally have two “remunerative aspects” that require scrutiny under the AKS: i) donor contributions , which the OIG stated can be analyzed as indirect remuneration to patients , and ii) financial assistance remuneration provided directly to patients. The OIG states that the AKS could be violated “if a donation is made to a PAP to induce the PAP to recommend or arrange for the purchase of the donor’s federally reimbursable items,” as well as if a PAP’s grant of financial assistance to a patient is made “to influence the patient to purchase (or induce the patient’s physician to prescribe) certain items.” [5]
Does CVC provide financial assistance?
In a letter dated January 4, 2018, the President and CEO of CVC announced that the charity would not offer financial assistance for any disease fund in 2018. [15] The decision left many patients who had previously received financial assistance from the charity suddenly without the ability to pay for necessary drugs in 2018, and caused concern in patients and even the government. On the same day as CVC’s announcement that it would not provide financial assistance in 2018, the OIG sent a letter to The Pharmaceutical Research and Manufacturers of America (“PhRMA”) about the “emergent issue” related to CVC, specifically that some patients would “face significant financial barriers to obtaining critical drugs” (“PhRMA Letter”). The PhRMA Letter stated that the OIG will not pursue administrative sanctions against any company that manufactures, sells, or distributes outpatient prescription drugs and provides free drugs during 2018 to federal health care program beneficiaries who were receiving assistance from CVC as of November 28, 2017, so long as certain outlined criteria are met. [16]
Does UT require a PAP review?
Unlike the Aegerion CIA, however, the UT CIA does not require the establishment of an independent PAP review program, and rather than requiring written agreements with PAPs to include certain provisions, the CIA requires UT to issue those guidelines as a policy for future interactions with PAPs. Recent IRS Scrutiny.
Where do patient assistance programs come from?
PAPs are most often sponsored by pharmaceutical companies. There are also state programs and nonprofit-sponsored programs.
How to sign up for a med program?
To sign up, you will either call the program or sign up online. You will need to submit forms like your taxes and residence status to prove your eligibility. Most programs also require your health provider to fill out a form. Once you apply and enroll, there may be limits on how much medication you can get or how long the program lasts.
Does GlaxoSmithKline offer assistance?
For example, GlaxoSmithKline offers an assistance program for its medications Benlysta and Nucala. Here, under their qualification section, they show what your maximum monthly gross income must be under, depending on your household size and where you live.
Can a patient assistance card help you?
Like manufacturer copay cards, patient assistance programs have received some criticism. But, they can and do help you if you are struggling to afford your medications. Keep reading to find out more about PAPs.
Do you have to pay for prescription drugs out of pocket?
And those without health insurance or adequate prescription drug coverage must pay for their medications out of pocket.
What is PAP in Medicare?
As explained in the Bulletin, arrangements through which a pharmaceutical manufacturer would use a PAP it operates or controls to subsidize its own products that will be payable by Medicare Part D present a heightened risk of fraud and abuse .
Can pharmaceutical companies make donations to PAPs?
For example, the Bulletin, reflecting long-standing OIG guidance, makes clear that pharma ceutical manufacturers can make cash donations to bona fide independent charity PAPs that are not affiliated with a manufacturer and operate without regard to donor interests, providing appropriate safeguards exist. These programs are typically operated by patient advocacy and support organizations.
Can OIG prevent Medicare from helping uninsured patients?
Finally, the Bulletin makes clear that nothing in any OIG laws or regulations prevents pharmaceutical manufacturers or others from helping uninsured patients and Medicare beneficiaries who have not enrolled in Part D with their outpatient prescription drugs.
What information should a PAP provider share with patients?
The company should also limit the information it shares about independent PAPs with patients and providers. For example, if the company’s reimbursement hub triages requests for co-pay or other financial assistance, the hub should provide only a general overview of the third-party assistance options to the patient or provider, along with contact information for each independent PAP that has an applicable fund and is currently accepting new applications (i.e., a “cold transfer”). Hub representatives should explicitly inform the patient or the patient’s provider that the referral to the independent PAP is not a guarantee of assistance and that the PAP has full discretion whether to provide assistance based on its own independent eligibility criteria. To this end, company personnel should generally be restricted from (a) filling out applications for patients or seeking information about the status of any individual application for assistance from any PAP, or (b) seeking detailed information regarding why and from which PAP any patients received or were denied assistance. In addition, the company should limit, as much as possible, the information coming from patients who were transferred to PAPs for assistance and who were denied or received assistance; if company personnel receive such information, they should not (1) share it beyond reimbursement support personnel, or (2) record it in the patient’s case notes.
What is the DOJ's interest in PAPs?
DOJ interest in drug company relationships with independent PAPs began in earnest in the midst of larger concerns regarding sharply rising drug prices. While investigating pricing schemes and specialty pharmacy relationships in 2015, DOJ began issuing subpoenas to pharmaceutical companies that manufacture expensive and specialty drugs that requested information on the companies’ relationships with independent PAPs. 9 Since then, the DOJ has broadened its inquiry to numerous pharmaceutical companies and independent PAPs.
What is a meaningful review and processing of funding requests?
Meaningful Review and Processing of Funding Requests: All requests should follow the company’s customary and generally applicable grant request processes, and these requirements should be incorporated within the PAP policy/procedure described above. The PAP policy/procedure should specify standardized, objective criteria for assessing requests from independent PAPs for both initial and additional or supplemental funding (e.g., funding beyond that which is set forth in the annual budget). Supplemental requests for funding must be reviewed for compliance with applicable Federal health care program requirements, OIG guidance, and company policies and procedures.
What are the restrictions on PAP data sharing?
Implementation of Data Sharing Restrictions: The company should take all necessary steps to ensure it does not receive (directly or indirectly through third parties) any data or information from the PAP that would enable the company to correlate the amount or frequency of its donations with support for its products or any related services. Such prohibited information may include individual patient information, or any information related to the identity, amount or nature of the products or services that are made available by the PAP from donations provided by the company, including any projections for additional funding required to continue a specific type of support. Within the company, the aggregate-level data received from independent PAPs should not be shared with commercial personnel.
Does a Hub representative have to inform the patient or the patient's provider that the referral to the independent PAP?
Hub representatives should explicitly inform the patient or the patient’s provider that the referral to the independent PAP is not a guarantee of assistance and that the PAP has full discretion whether to provide assistance based on its own independent eligibility criteria.
Is it permissible for a charitable organization partly funded by kidney dialysis providers to pay Medicare Part B?
4 See OIG Adv. Op. 97-01 (June 11, 1997) (advising that it is permissible for a charitable organization partly funded by kidney dialysis providers to pay Medicare Part B, Medigap and other health insurance premiums for end-stage renal disease patients who are financially needy).
Is PAP independent?
Independence of PAP with Respect to Patient Eligibility: The company may not ex ert (directly or through any affiliate) any influence or control over the independent PAP’s process or criteria for determining eligibility of patients who qualify for assistance. Part Three: A Developing Risk Area — Free Drug Programs.
How many patient assistance programs are there in 2018?
Design, Setting, and Participants Descriptive cross-sectional study of the 6 largest independent charities offering patient assistance programs for patients including, but not limited to, Medicare beneficiaries in 2018. These charities offered 274 different disease-specific patient assistance programs. Drugs were identified for subgroup analysis that had any use reported on the Medicare Part D spending dashboard and any off-patent brand-name drugs that incurred more than $10 000 in Medicare spending per beneficiary in 2016.
What are the primary outcomes of patient assistance programs?
Main Outcomes and Measures The primary outcomes were the characteristics of patient assistance programs, including assistance type, insurance coverage (vs uninsured), and income eligibility. The secondary outcomes were the cost of the drugs covered by the patient assistance programs and the coverage of expensive off-patent brand-name drugs vs substitutable generic drugs.
How much did Medicare Part D spend in 2016?
In the drug-level analysis, the median 2016 Medicare Part D spending per beneficiary was $1157 for medications covered by these programs compared with $367 for the medications not covered.
Why are uninsured patients excluded from Medicare?
The programs often featured the number of insured patients as an important performance metric. 25, 26 Because covering an insured patient requires less money compared with covering an uninsured patient who needs the same drug, one possible explanation for excluding uninsured patients is that the programs attempted to use their limited funding to assist as many beneficiaries as possible. The study also found that 46% of the patient assistance programs provided insurance premium assistance, which by design is not applicable to uninsured patients. Taken together, enhancing patient assistance programs to include uninsured patients, who are likely to face greater affordability challenges than insured patients, may be an area for improvement.
Why is patient assistance important?
For patients taking expensive drugs, some patient assistance programs may play an important part in defraying the cost of needed medications. These patients may have difficulty affording their medications when they do not have health insurance coverage for the drugs, when they are in the deductible phase of the benefit, or when they reach the coverage gap (the period in which they are required to pay a larger share of total drug costs). This is especially a problem for Medicare enrollees who are prescribed high-cost specialty drugs because most Medicare Part D plans charge higher coinsurance for these specialty drugs and there is no catastrophic cap in the Medicare program. Thus, out-of-pocket costs can reach thousands of dollars. 24 For this reason, independent charity foundations offering patient assistance programs to these patients are entitled to receive tax-deductible donations from pharmaceutical companies. However, the findings from this study suggest that several features of the programs may limit their usefulness to financially needy patients and bolster the use of expensive drugs.
How does patient assistance work?
Patient assistance programs help patients afford prescription drugs by subsidizing their out-of-pocket costs. Federal health programs, including Medicare, prohibit the use of manufacturer-sponsored drug-specific patient assistance programs due to the federal Anti-Kickback Statute that forbids manufacturers from offering any remuneration for a federally reimbursable item. 1 However, federal health programs allow patients to participate in disease-specific independent charity patient assistance programs based on the assumption that these programs do not violate anti-kickback laws. 2 Pharmaceutical companies may make tax-deductible donations to these disease-specific funds.
What is the eligibility criteria for patient assistance?
Eligibility for all of the patient assistance programs was based on the following criteria: annual household income measured by the federal poverty level (FPL) guidelines, insurance status, physician endorsement, prescription information, and proof of receiving treatment in the United States.